Insured members of the AARP Medicare Supplement Insurance Plans from UnitedHealthcare and the Dentegra network access program

For providers
Over 3.5 million seniors are looking for you
Gain patients and help advance senior oral health with a simple way to serve insured members covered under an AARP® Medicare Supplement Insurance Plan from UnitedHealthcare.
One of our network access plans
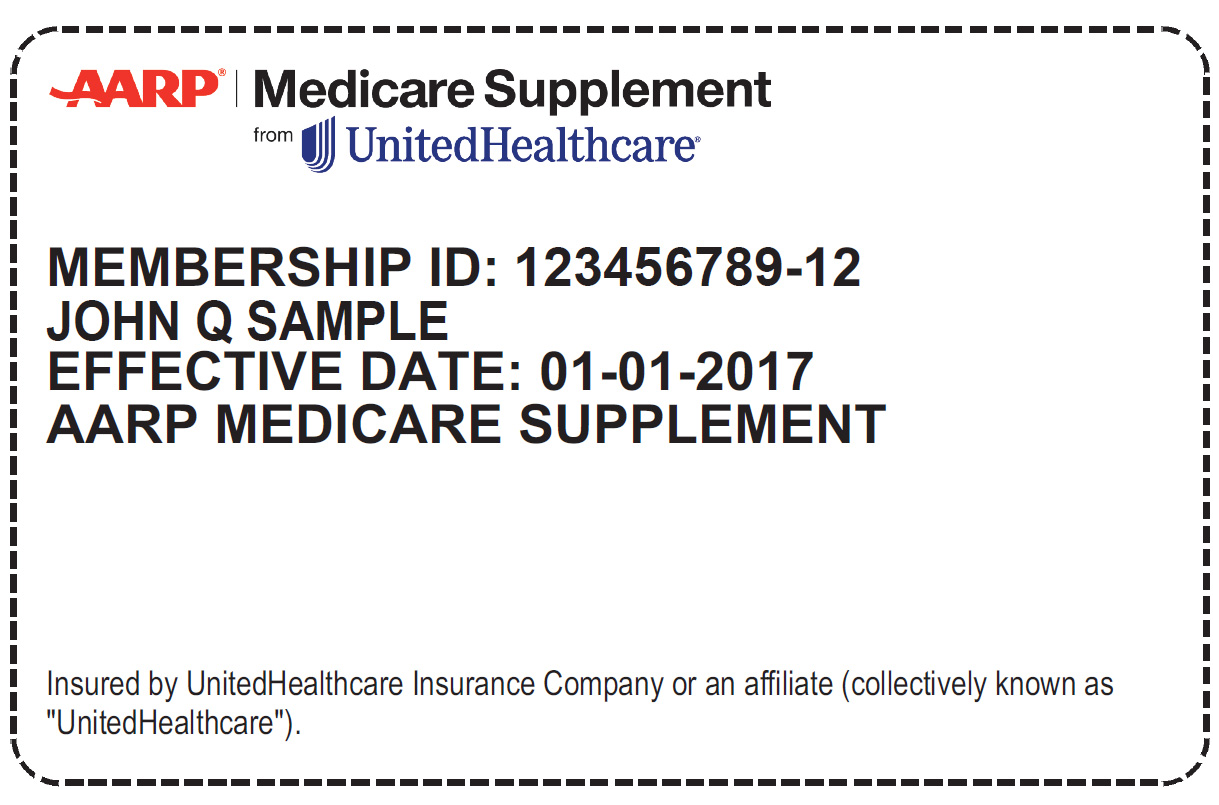
AARP Medicare Supplement Insurance plan holders (over 3.5 million and counting!) only need to visit a provider in the Dentegra network, show their AARP Medicare Supplement plan ID card and pay you the Dentegra contracted fee.
Patients covered under these plans may contact your office and ask about the "Dentegra discount" or "discount plan," which is our network access plan (it's even easier!).
How it works
The Dentegra contracted fee (the "Dentegra discount") that AARP Medicare Supplement plan holders pay you is not dental insurance. That means you don't need to research benefits, submit claims or wait to be paid. Here's all you need to do.
- Check the patient's AARP Medicare Supplement Insurance plan ID card
- Provide the necessary dental care
- Charge your contracted Dentegra fee
That's it!
Questions?
If you're not sure where to find your Dentegra fee schedule or you have other questions, contact our Network Development team at 866-238-1580. You can also email providerinfo@dentegra.com.
